Minimally Invasive Surgery (MIS) Sacroiliac (SI) Joint Fusion
Minimally Invasive Surgery (MIS) Sacroiliac (SI) Joint Fusion is a surgical procedure designed to stabilize the sacroiliac joint, which connects the spine to the pelvis. This joint can become a source of chronic pain due to conditions such as sacroiliitis, degenerative arthritis, post-pregnancy, as a result of trauma, or after prior spinal fusion. MIS SI Joint Fusion is a less invasive alternative to traditional open surgery, offering reduced recovery times and minimized tissue disruption.
Why is Minimally Invasive SI Joint Fusion Surgery Considered Controversial?
The evidence base for Minimally Invasive SI Joint fusion is continually growing and is supported by high quality (Randomised Control Trial) data. Nonetheless, this procedure is controversial by many surgeons for several reasons:
Lack of Consensus on Diagnosis: SI joint dysfunction is often difficult to diagnose accurately because its symptoms can overlap with other conditions, such as lumbar spine issues or hip problems. The effectiveness of the surgery relies on an accurate diagnosis, but the criteria for diagnosing SI joint dysfunction are not universally agreed upon, leading to concerns about whether the right patients are being selected for surgery.
Limited Long-term Data: While several studies show promising short-term results for pain relief and improved function, there is limited long-term data on the durability and outcomes of minimally invasive SI joint fusion. Concerns exist about whether the benefits seen in the short term will persist over the long term.
Variability in Surgical Techniques and Devices: The minimally invasive approach includes various techniques and devices, and not all of them have the same level of evidence supporting their use. This variability can lead to inconsistent outcomes, with some patients experiencing significant improvement and others seeing little to no benefit.
Potential for Complications: Although minimally invasive, the procedure is technically challenging, and should only be performed by surgeons specifically trained in this technique. The procedure carries risks, including infection, nerve injury, implant migration, or continued pain.
Perception of Inconsistent Outcomes: While most patients report significant pain relief after the procedure, some experience little to no improvement or even worsening of symptoms. There are many factors that can contribute to this including misdiagnosis. This inconsistency fuels the debate about whether the procedure is genuinely effective or if the success rates are overestimated.
These factors contribute to the ongoing debate in the medical community about the appropriate use and long-term value of minimally invasive SI joint fusion. The evidence to support Minimally Invasive SI Joint Fusion and recommendations can be summarized on the National Institute of Clinical Health and Care Excellence (NICE – UK) here: https://www.nice.org.uk/guidance/ipg578/chapter/1-Recommendations
What Happens During MIS SI Joint Fusion Surgery?
Preparation
- Hospital Admission: You will be admitted to the hospital on the day of surgery. Fasting is required before the procedure, as directed by your anaesthetist.
- Anaesthesia: The surgery is performed under general anaesthesia, ensuring you are asleep and pain-free throughout the procedure.
Surgical Approach
- Patient Positioning: You will be positioned prone (face down) to allow A/Prof Buckland access to the SI joint.
- Incision: A small incision (typically less than 2 inches) is made over side of the affected hip, and the gluteal muscles are separated but not divided with the use of specialised retractors.
Joint Preparation & Implant Placement
Accessing the SI Joint: A/Prof Buckland uses computer navigation and fluoroscopy (real-time X-ray) to guide the surgical instruments and ensure accurate implant placement. 2-3 guide-wires (pins) are placed across the joint and the position confirmed with X-ray.
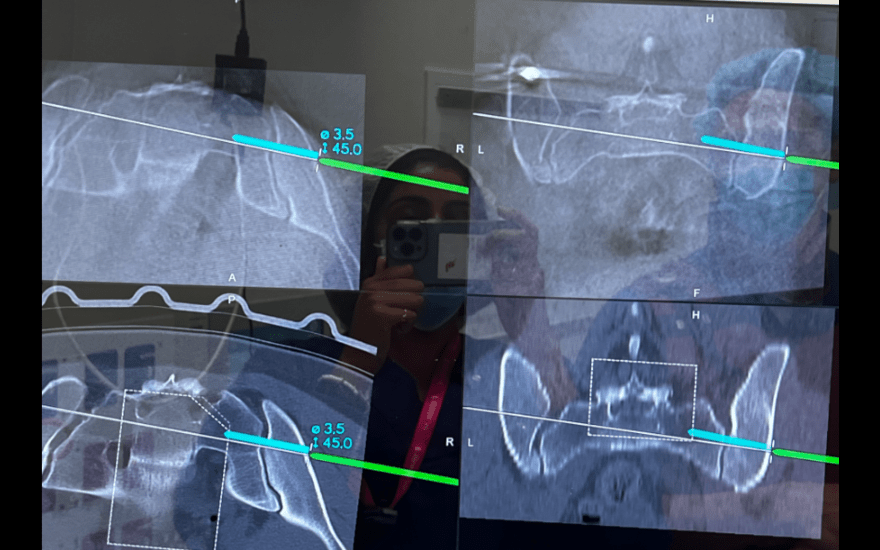
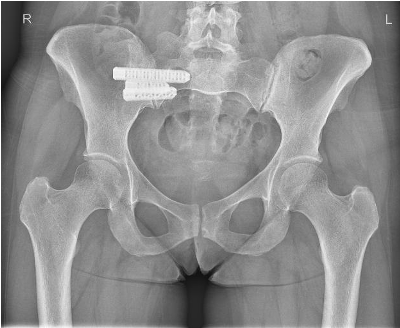
Implant Placement: Instruments are placed over the guide-wires in order to prepare the joint and adjacent bone of the pelvis and sacrum for passage of the definitive implants. Once the preparation is done the definitive Titanium implants are placed over the guide-wires, and the guidewires are removed. Implant position is confirmed by obtaining 3D X-ray images prior to leaving the operating room.
Closure
- The small incision is closed with sutures or surgical staples, and a sterile dressing is applied to protect the wound. The surrounding tissues are repositioned to minimize the risk of complications.
Postoperative Care and Recovery
Hospital Stay
Most patients can go home the following day after surgery, depending on their recovery progress and overall health.
Pain Management
Pain is managed with medications, and early mobilization is encouraged to reduce the risk of complications such as blood clots or pneumonia. MIS techniques generally result in less postoperative pain compared to traditional open surgery.
Rehabilitation
Physicotherapy: A tailored rehabilitation program will be initiated shortly after surgery. Early physical therapy focuses on gentle exercises to maintain mobility without stressing the SI joint. As healing progresses, more vigorous activities will be introduced to strengthen the muscles supporting the SI joint.
Activity Restrictions and Weight-bearing Status: You will need crutches for the first 6 weeks after surgery, and can put only part of your weight through the affected side over this time. You should avoid heavy lifting, bending, and twisting for 3 months after surgery. Gradual return to normal activities will be guided by your healthcare team.
Follow-up
Follow-up appointments will be scheduled typically at 2 weeks, 6 weeks, 3 Months, 6 Months and 12 Months after surgery. X-rays are obtained all of these visits other than 2 weeks post-surgery.
Risks and Complications
As with any surgery, there are potential risks, including:
- Infection: There is a small risk of infection at the surgical site.
- Bleeding: While rare, excessive bleeding during or after surgery is possible.
- Nerve Injury: There is a risk of injury to the nearby nerves, which could result in weakness, numbness, or other neurological symptoms.
- Non-Union: In some cases, the bones may not fuse as expected, potentially requiring additional surgery.
- Implant Issues: There may be complications related to the implants, such as loosening or misplacement.
Patient-Reported Outcomes and Results
Minimally Invasive SI Joint Fusion significantly improves function and pain in the majority of patients. The following literature provides the highest-quality data supporting this technique and patient-reported outcomes.
Learn more about A/Prof Buckland’s patient-reported outcomes of MIS SI Joint Fusion here.
Publications
Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction
Polly DW, Swofford J, Whang PG, Frank CJ, Glaser JA, Limoni RP, Cher DJ, Wine KD, Sembrano JN, and the INSITE Study Group.
Int J Spine Surg. 2016;10:Article 28.
Predictors of Outcome in Conservative and Minimally Invasive Surgical Management of Pain Originating from the Sacroiliac Joint – A Pooled Analysis
Dengler J, Duhon B, Whang P, Frank C, Glaser J, Sturesson B, Garfin S, Cher D, Rendahl A, Polly D, on behalf of the INSITE, iMIA and SIFI study groups.
Spine. 2017;42(21):1664-1673.