Adult Spinal Deformity Correction
Adult spinal deformity correction is a complex and multifaceted surgical procedure designed to address abnormal curvatures or malalignment in the spine. This type of surgery is typically considered for individuals who experience significant pain, functional impairment, or neurological symptoms due to their spinal deformity. The process involves several key steps:
Preoperative Evaluation
- Clinical Assessment: A thorough medical history and physical examination are conducted to assess the severity of the deformity, associated symptoms, and overall health.
- Imaging Studies: X-rays, MRIs, and CT scans are used to evaluate the spine’s structure, alignment, and any underlying issues such as spinal stenosis, disc degeneration, or nerve compression. Your bone density is assessed and may require optimization prior to surgery.
- Functional Testing: This may include nerve conduction studies or other tests to assess the impact of the deformity on the nervous system and overall function.
- Risk Assessment: Evaluating the patient’s fitness for surgery, including cardiac, pulmonary, and other systemic considerations. Any medical problems will be optimized prior to surgery to reduce the risk of perioperative complications.
Surgical Planning
- Correction Strategy: The surgical plan is tailored to the individual’s specific deformity, considering the type and extent of curvature (e.g., scoliosis, kyphosis), the patient’s age, bone quality, and overall health.
- Type of Surgery: Options may include a combination of spinal fusion, osteotomy (removal of a section of bone), laminectomy (removal of part of a vertebra), and implantation of rods, screws, and other hardware to stabilize and correct the spine.
- Alignment Goals: The goal is to restore your alignment based upon your age, functional goals and your individual body shape. In addition, the surgery aims to relieve nerve compression, and improve posture and function.
Surgical Procedure
- Anesthesia: General anesthesia is used.
- 1-Stage vs 2-Stage Surgery: Depending on the specific deformity, patient comorbidities and procedural complexity, the surgery may be performed under one anaesthetic (1-Stage) or under two separate anaesthetics a few days apart (2-Stage). A/Prof Buckland will counsel you on the specific procedure plan prior to the surgery.
- Spinal Cord Monitoring: Spinal cord monitoring is used throughout the surgery in order to detect any stress on the spinal cord, and allow changes to the surgical plan in ‘real-time’. Small needles are placed in the scalp and muscle groups of the arms and legs to allow detection of any abnormalities.
- Incision: Depending on the approach (anterior, posterior, or combined), A/Prof Buckland makes one- or several- incisions to access the spine.
- Instrumentation of the Spine: Screws, hooks or tapes will be placed in each vertebra in order to allow manipulation of the bones individually. The screws are placed using computer navigation assistance to increase accuracy, improve safety and reduce operation time.
- Correction and Stabilization: A/Prof Buckland corrects the deformity by realigning the spine and stabilizing it using metal rods, screws, or other implants such as cages. Bone grafts are be placed to promote fusion between vertebrae which come from your own local bone (local autograft), bone from the back of the pelvis (iliac crest bone graft) or from a bone tissue donor (allograft).
- Decompression: If necessary, parts of the vertebrae or intervertebral discs are removed to relieve pressure on the spinal cord or nerves.
- Intraoperative X-rays: X-rays are taken in the operating room before the procedure is completed to ensure accurate placement of implants, and that the alignment has been appropriately corrected.
Case 1
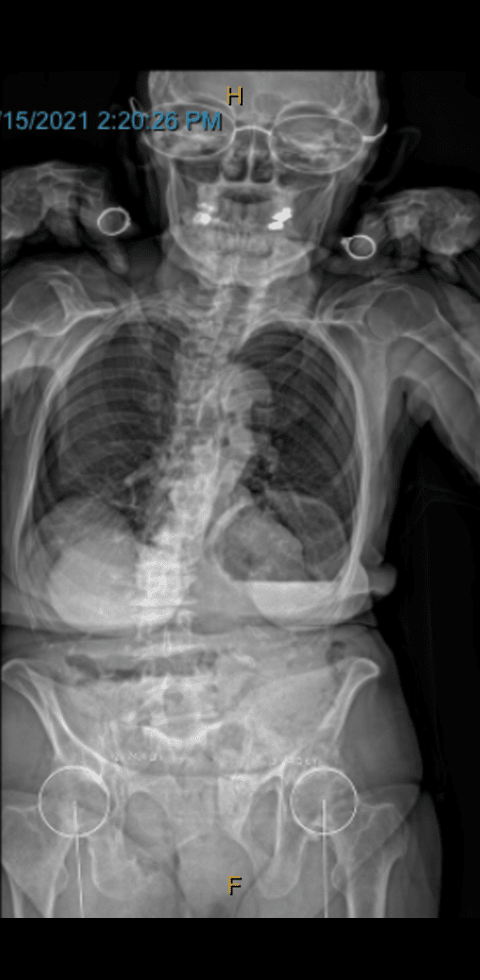
Pre Op AP X-Ray
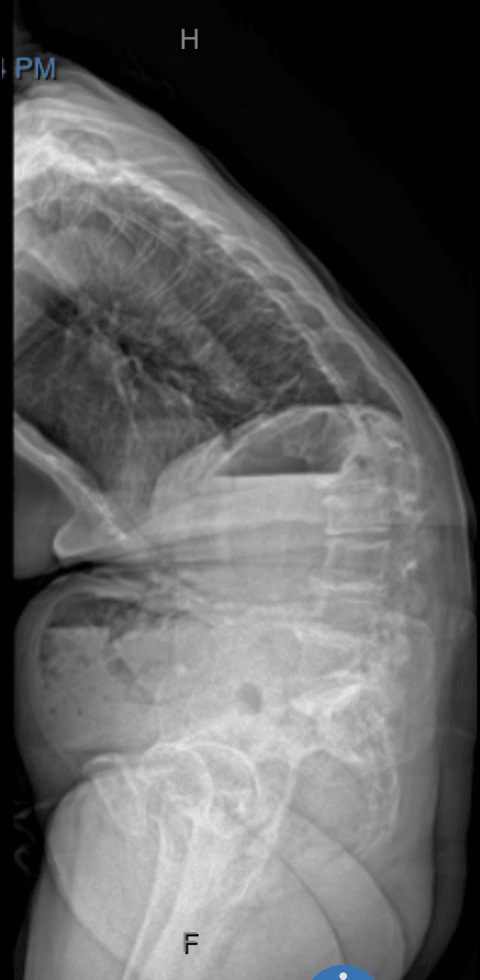
Pre Op Lateral X-Ray
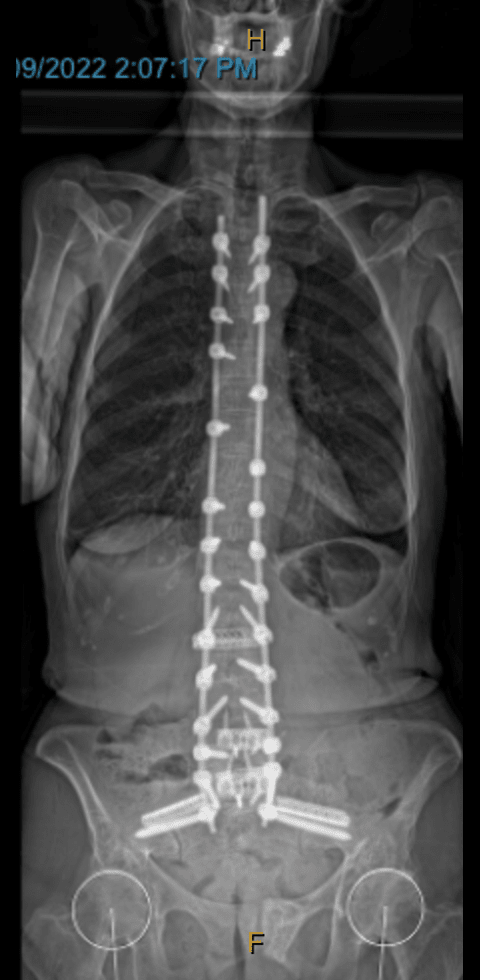
Post Op Ap X-Ray

Post Op Lateral X-Ray
Case 2

Pre Op AP X-Ray

Pre Op Lateral X-Ray

Post Op Ap X-Ray

Post Op Lateral X-Ray
Risks and Complications
Adult spinal deformity correction has an almost 100% complication rate. Fortunately, 80% of these complications are relatively minor and small “bumps” along the road to recovery. Some of these include minor wound problems or a urinary tract infection etc.
Unfortunately, 20% of the time, these complications may be significant complications such as:
- Infection: As with any surgery, there is a risk of infection.
- Hardware Issues: There may be complications related to the implanted hardware, such as breakage or loosening.
- Junctional Kyphosis or Fracture: Postural decline may occur after spinal re-alignment due to ligament failure or fracture above (Proximal Junction) or below (Distal Junction) the fused segment of the spine. This may require additional surgeries.
- Non-union: In some cases, the bones may not fuse as intended, leading to a need for additional surgery.
- Neurological Complications: There is a risk of nerve or spinal cord damage, which can result in weakness, numbness, or other neurological symptoms.
- Blood Clots: Patients are at risk for developing blood clots, particularly in the legs (deep vein thrombosis).

Postoperative Care
- Hospital Stay: The patient typically stays in the hospital for several days to a week, depending on the complexity of the surgery. Inpatient rehabilitation may be required depending on the procedure complexity, medical comorbidities and social supports. This will be planned by A/Prof Buckland’s treating team during your inpatient stay.
- Pain Management: Pain is managed with medications, and the patient may begin physical therapy while still in the hospital. Pain control can be challenging in the first few days after surgery, particularly in people who have used a lot of pain relief (opiates) prior to surgery. A specialist pain management doctor will typically work as part of the treating team to ensure that our best efforts are made to control your pain appropriately. The aim is to treat the pain to a level that allows you to mobilise, not to prevent mobility in an effort to avoid pain.
- Rehabilitation: Ongoing physical therapy and rehabilitation are critical to recovery. The patient will gradually return to normal activities under the guidance of healthcare providers. A brace may be recommended in the first 3 months post-surgery.
- Follow-up: Regular follow-up visits are necessary to monitor the healing process, check your implants with x-rays, guide your physiotherapy and activity levels and manage your pain or any complications.
Patient Outcomes
- Pain Relief and Function: Successful surgery often leads to significant pain relief and improved function, though some residual symptoms may persist.
- Lifestyle Modifications: Patients may need to make lifestyle changes to protect their spine and maintain the surgical results. It is important to know that the cost of restoring alignment and reducing pain is that flexibility is reduced. You may need ‘work-arounds’ for daily activities such as putting on shoes and socks, dressing yourself and personal hygiene depending on the extent of fusion required.
- Ongoing Monitoring: Regular monitoring is required to ensure proper healing and function, especially in the first few years after surgery.
This surgery is generally reserved for cases where non-surgical treatments have failed and the spinal deformity significantly impacts the patient’s quality of life. Before proceeding, patients should have a detailed discussion with A/Prof Buckland about the potential benefits, risks, and recovery process.