Single-Position Lumbar Fusion
Single-position lumbar fusion surgery is an advanced surgical technique that allows both the anterior and posterior aspects of the spine to be accessed and treated without needing to reposition the patient during the procedure. This approach is designed to improve efficiency, reduce surgical time, and enhance patient outcomes while reducing complications.
Why Choose Single-Position Lumbar Fusion?
This technique is particularly beneficial for patients requiring spinal fusion at multiple levels or those who need both anterior and posterior surgical approaches. Posterior fusion techniques have lower fusion rates that fusion of both the anterior (front) and posterior (back) columns of the spine together. Traditionally, anterior-posterior lumbar fusion often required repositioning the patient during surgery, which can increase the duration of the operation and the risks associated with prolonged anaesthesia. Single-position surgery combines all the benefits of minimally invasive fusion, while providing gold-standard fusion rates and alignment restoration.
What Happens During Single-Position Lumbar Fusion Surgery?
Preparation
Hospital Admission: You will be admitted on the day of surgery and required to fast prior to the procedure, as instructed by your anaesthetist.
Anaesthesia: The surgery is performed under general anaesthesia, ensuring you are asleep and pain-free during the entire procedure.
Surgical Approach
Patient Positioning: The patient is positioned in a lateral decubitus (side-lying) position, or in a prone (face down) depending on the specific goals of the surgery. This positioning allows A/Prof Buckland to access both the anterior (front) and/or lateral (side) and/or posterior (back) aspects of the lumbar spine without needing to reposition the patient.

Anterior/Lateral Lumbar Access
Incision: A small incision is made on the side of the abdomen to access the lumbar spine from the front. The access to the spine is made without needing to divide any muscles, and may be performed with the assistance of a Vascular Surgeon, depending on the disc level.
Disc Removal: The damaged or degenerated disc is removed, and any necessary bone spurs or other structures compressing the nerves are addressed.
Insertion of Cage and Bone Graft: A cage (spacer) filled with bone graft material is placed in the disc space to restore disc height and facilitate fusion between the vertebrae. This helps to relieve pressure on the nerves and stabilize the spine.
Posterior Lumbar Access
Incision and Exposure: Without repositioning the patient, A/Prof Buckland then accesses the posterior part of the spine through two small incisions on the back.
Screw and Rod Placement: Pedicle screws and rods are inserted into the vertebrae using computer assisted navigation technology to stabilize the spine and promote fusion. The implants are typically made of titanium.
Decompression: If necessary, additional decompression procedures, such as laminectomy or foraminotomy, are performed to relieve pressure on the spinal nerves via the incision used for placing the screws.
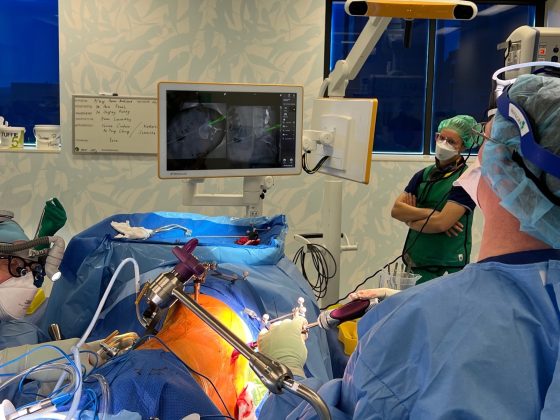
A/Prof Buckland (right) places computer-navigated pedicle screws while Mr Domenic Robinson (Vascular Surgeon (Left)) performs the anterior (front) exposure.
Closure
The surgical wounds are closed with sutures, and sterile dressings are applied to protect the incision sites. The image on the right shows surgical scars two weeks after single-position lumbar fusion.
Postoperative Care and Recovery
Hospital Stay
Most patients stay in the hospital for 1-3 days following single-position lumbar fusion surgery, depending on the extent of the surgery and individual recovery progress.
Pain Management
Pain is managed with medications, and early mobilization is encouraged to minimize complications like blood clots or pneumonia. Patients typically experience less postoperative pain due to the minimally invasive nature of the surgery. Most patients are able to cease pain medications within 2-4 weeks after surgery.
Outpatient Rehabilitation
Physiotherapy: A rehabilitation program tailored to your specific needs will be initiated shortly after surgery. This will focus on restoring strength, flexibility, and proper body mechanics.
Activity Restrictions: Patients should avoid heavy lifting, bending, and twisting for at least 3 months after surgery. Gradual return to normal activities is guided by A/Prof Buckland’s team at follow-up visits.
Follow-up
Follow-up appointments will be scheduled to monitor your recovery, typically at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months post-surgery.
Patient-Reported Outcomes and Results
Lumbar Fusion Surgery significantly improves function and pain in the majority of patients. Learn more about A/Prof Buckland’s patient-reported outcomes of 1-2 level lumbar fusion below.
A/Prof Buckland has published extensively in the field of single-position surgery, including the demonstrated benefits. The following publications are available for review of this technique.
- Technique, Safety, and Accuracy Assessment of Percutaneous Pedicle Screw Placement Utilizing Computer-Assisted Navigation in Lateral Decubitus Single-Position Surgery. Calek AK, Hochreiter B, Buckland AJ.Int J Spine Surg. 2024 Jul 18:8613. doi: 10.14444/8613. Online ahead of print.PMID: 39025526
- Lateral lumbar interbody fusion at L4-L5 has a low rate of complications in appropriately selected patients when using a standardized surgical technique. Buckland AJ, Huynh NV, Menezes CM, Cheng I, Kwon B, Protopsaltis T, Braly BA, Thomas JA.Bone Joint J. 2024 Jan 1;106-B(1):53-61. doi: 10.1302/0301-620X.106B1.BJJ-2023-0693.R2.PMID: 38164083
- Single-Position Prone Lateral Lumbar Interbody Fusion Increases Operative Efficiency and Maintains Safety in Revision Lumbar Spinal Fusion. Buckland AJ, Proctor DJ, Thomas JA, Protopsaltis TS, Ashayeri K, Braly BA.Spine (Phila Pa 1976). 2024 Feb 1;49(3):E19-E24. doi: 10.1097/BRS.0000000000004699. Epub 2023 Apr 27.PMID: 37134133
- Lateral decubitus single position anterior posterior surgery improves operative efficiency, improves perioperative outcomes, and maintains radiological outcomes comparable with traditional anterior posterior fusion at minimum 2-year follow-up. Buckland AJ, Braly BA, O’Malley NA, Ashayeri K, Protopsaltis TS, Kwon B, Cheng I, Thomas JA.Spine J. 2023 May;23(5):685-694. doi: 10.1016/j.spinee.2023.01.001. Epub 2023 Jan 12.PMID: 36641035
- Single-position circumferential lumbar spinal fusion: an overview of terminology, concepts, rationale and the current evidence base. Thomas JA, Menezes C, Buckland AJ, Khajavi K, Ashayeri K, Braly BA, Kwon B, Cheng I, Berjano P.Eur Spine J. 2022 Sep;31(9):2167-2174. doi: 10.1007/s00586-022-07229-4. Epub 2022 Aug 1.PMID: 35913621
- Spinal exposure for anterior lumbar interbody fusion (ALIF) in the lateral decubitus position: anatomical and technical considerations. Buckland AJ, Leon C, Ashayeri K, Cheng I, Alex Thomas J, Braly B, Kwon B, Maglaras C, Eisen L.Eur Spine J. 2022 Sep;31(9):2188-2195. doi: 10.1007/s00586-022-07227-6. Epub 2022 May 12.PMID: 35552530 Review.
- Lateral decubitus single position anterior-posterior (AP) fusion shows equivalent results to minimally invasive transforaminal lumbar interbody fusion at one-year follow-up. Ashayeri K, Alex Thomas J, Braly B, O’Malley N, Leon C, Cheng I, Kwon B, Medley M, Eisen L, Protopsaltis TS, Buckland AJ.Eur Spine J. 2022 Sep;31(9):2227-2238. doi: 10.1007/s00586-022-07226-7. Epub 2022 May 13.PMID: 35551483
- Setting for single position surgery: survey from expert spinal surgeons. Guiroy A, de Andrada-Pereira B, Camino-Willhuber G, Berjano P, Lamartina C, Buckland AJ, Gagliardi M, Khajavi K, Turner JD, Thomas JA, Menezes C, Lehman R Jr, Uribe J, Asghar J.Eur Spine J. 2022 Sep;31(9):2239-2247. doi: 10.1007/s00586-022-07228-5. Epub 2022 May 7.PMID: 35524824
- Anterior column reconstruction of the lumbar spine in the lateral decubitus position: anatomical and patient-related considerations for ALIF, anterior-to-psoas, and transpsoas LLIF approaches. Buckland AJ, Ashayeri K, Leon C, Cheng I, Thomas JA, Braly B, Kwon B, Eisen L.Eur Spine J. 2022 Sep;31(9):2175-2187. doi: 10.1007/s00586-022-07127-9. Epub 2022 Mar 2.PMID: 35235051
- Single position lateral decubitus anterior lumbar interbody fusion (ALIF) and posterior fusion reduces complications and improves perioperative outcomes compared with traditional anterior-posterior lumbar fusion. Ashayeri K, Leon C, Tigchelaar S, Fatemi P, Follett M, Cheng I, Thomas JA, Medley M, Braly B, Kwon B, Eisen L, Protopsaltis TS, Buckland AJ.Spine J. 2022 Mar;22(3):419-428. doi: 10.1016/j.spinee.2021.09.009. Epub 2021 Sep 30.PMID: 34600110
- Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Buckland AJ, Ashayeri K, Leon C, Manning J, Eisen L, Medley M, Protopsaltis TS, Thomas JA.Spine J. 2021 May;21(5):810-820. doi: 10.1016/j.spinee.2020.11.002. Epub 2020 Nov 13.PMID: 33197616