Patient Outcome Data
As part of your standard of care, A/Prof Buckland gathers patient reported outcomes (PROs) in order to ensure we gain clear insights into the success rates of our surgeries. By sharing real patient experiences and outcomes, we aim to build trust and confidence in our procedures, helping you make informed decisions about your healthcare journey. This data not only aids in continuous improvement but also guides others towards achieving their best possible outcomes.
Disclaimer: The results presented herein are representative only of A/Prof Buckland’s surgical outcomes and experiences. They are specific to the techniques and practices of A/Prof Buckland and cannot be generalized to represent the results of other surgeons. Individual patients’ outcomes may vary based on a variety of factors, including but not limited to the specific methods used, patient health conditions, and procedural circumstances.
Microdiscectomy / Laminotomy
Baseline |
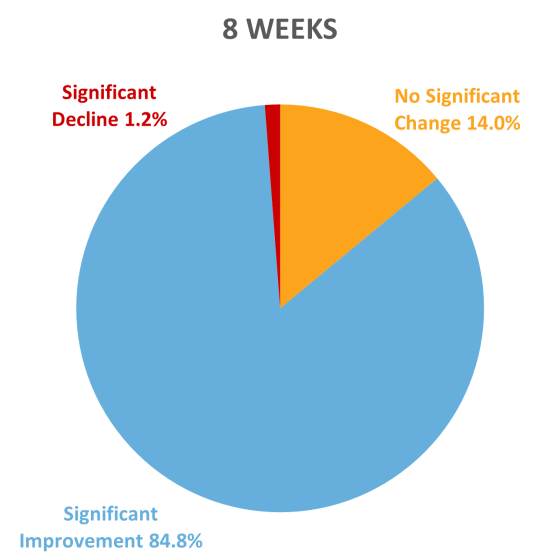
8 weeks |
1YR |
2YR |
|
ODI |
42.2 |
18.4 |
13.9 |
12.3 |
1-2 Level Decompression
Decompressions include Laminectomy Laminotomy and Microdiscectomy
Baseline |
8 weeks |
1YR |
2YR |
|
ODI |
42.2 |
18.4 |
13.9 |
12.3 |

Interpretation of ODI scores
0 to 20: minimal disability: The patient can cope with most living activities. Usually no treatment is indicated apart from advice on lifting sitting and exercise.
21-40: moderate disability: The patient experiences more pain and difficulty with sitting, lifting and standing. Travel and social life are more difficult and they may be disabled from work. Personal care, sexual activity and sleeping are not grossly affected and the patient can usually be managed by conservative means.
41-60: severe disability: Pain remains the main problem in this group, but activities of daily living are affected. These patients require a detailed investigation.
61-80: crippled: Back pain impinges on all aspects of the patient’s life. Positive intervention is required.
81-100: These patients are either bed-bound or exaggerating their symptoms.
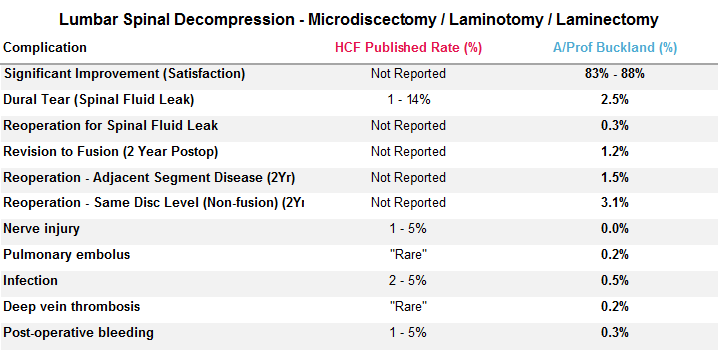
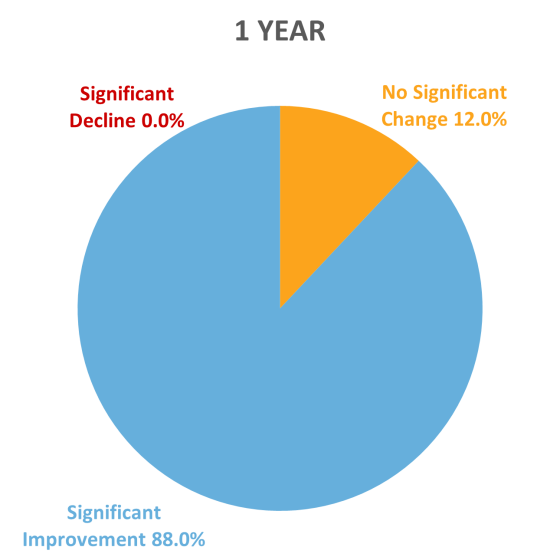
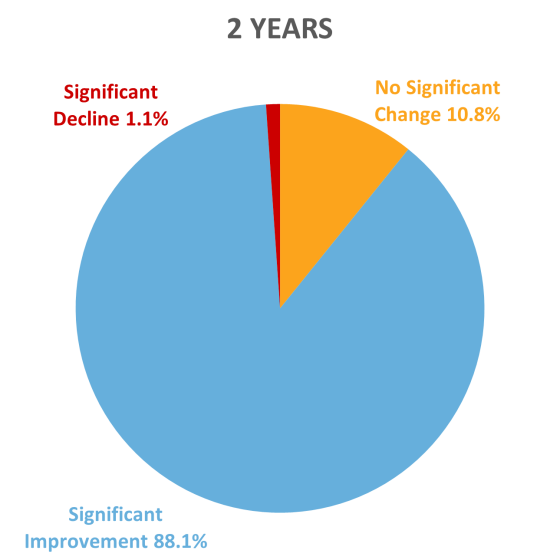
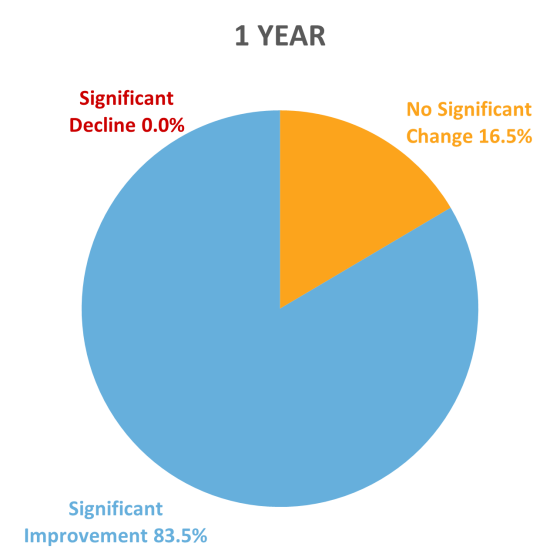
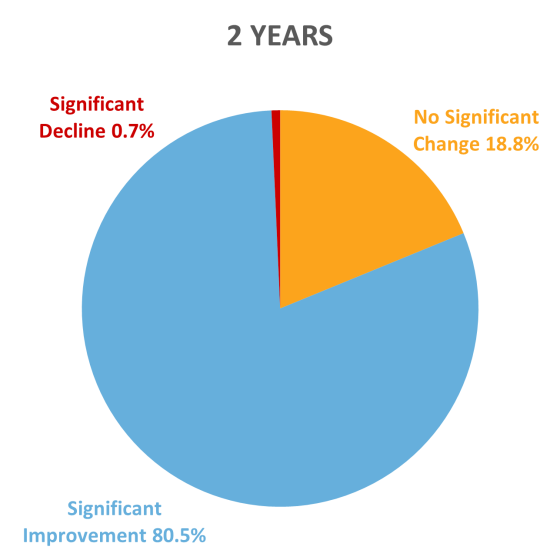
How do we measure clinical improvement?
Clinical improvement is measured by the ‘Minimally Clinically Important Difference’ (MCID). This measurement is used to determine the change in function that a patient would recognise as beneficial and meaningful.
MCID is measured as an improvement in Oswestry Disability Index (ODI) of more than 12.8 percent1.
- Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and Pain Scales. The Spine Journal. 2008;8(6):968-974