Mid Foot Arthritis
Anatomy of the Midfoot
The midfoot is composed of several small joints that connect the forefoot (the toes and metatarsal bones) to the hindfoot (the heel and ankle bones). These joints, including the tarsometatarsal (TMT) joints, are essential for the stability and function of the foot, allowing for proper weight distribution during walking, running, and standing. In a healthy foot, these joints move smoothly due to the presence of cartilage, which cushions the bones and absorbs shock.
What is Midfoot Arthritis?
Midfoot arthritis occurs when the cartilage in the midfoot joints degenerates, leading to pain, stiffness, and inflammation. The condition may develop spontaneously, following trauma (such as a fracture or dislocation), or in association with inflammatory diseases like rheumatoid arthritis. Over time, the joint space narrows, bone spurs may form, and the joints become less flexible, causing discomfort and difficulty with daily activities.

What Happens in Midfoot Arthritis?
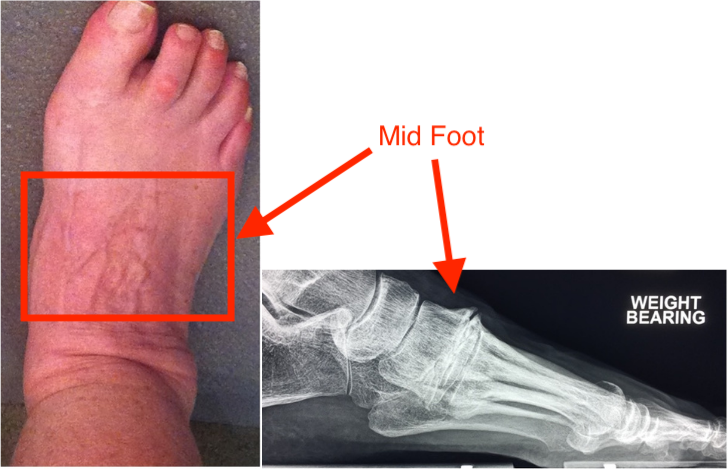
In midfoot arthritis, the smooth cartilage lining the joints gradually wears away, leading to increased friction between the bones. This degeneration results in pain, swelling, and the development of bone spurs, which can cause a visible lump on top of the foot. This lump may rub against shoes, causing additional discomfort. Patients often experience pain on the top of the foot, midway between the toes and the ankle, though the pain may be difficult to pinpoint exactly.
Midfoot arthritis can significantly affect mobility, and symptoms may worsen with activities that involve standing, walking, or wearing tight shoes.
Symptoms of Midfoot Arthritis
- Pain in the middle of the foot, often felt on the top of the foot.
- Stiffness in the midfoot, particularly in the morning or after periods of rest.
- Swelling and tenderness over the midfoot joints.
- A noticeable lump or bone spur on the top of the foot.
- Difficulty walking or standing for extended periods.
- Pain that worsens with physical activity or when wearing tight or ill-fitting shoes.
How is Midfoot Arthritis Diagnosed?
Diagnosis of midfoot arthritis is based on a combination of clinical examination and imaging studies. The key components of diagnosis include:
Physical Examination: The physician will evaluate the foot for pain, swelling, and reduced range of motion in the midfoot joints. They may also assess for the presence of bone spurs.
Imaging: X-rays are typically used to assess joint space narrowing, bone spur formation, and overall degeneration in the midfoot joints. In some cases, further imaging such as a CT scan or MRI may be recommended to evaluate the extent of damage.
How is Midfoot Arthritis Treated?
Treatment for midfoot arthritis aims to relieve pain, improve mobility, and preserve the function of the foot. Non-surgical treatments are generally attempted first, with surgery reserved for more severe cases.
Non-Surgical Treatment
- Supportive Footwear and Insoles: Wearing supportive shoes that provide adequate cushioning and arch support can help relieve pressure on the midfoot joints. Custom orthotics (shoe inserts) may be prescribed to improve foot alignment and reduce pain.
- Physiotherapy: Physical therapy, including exercises that stretch the calf muscles and improve joint flexibility, can be helpful in reducing pain and stiffness.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may be used to reduce inflammation and pain.
- Activity Modification: Avoiding high-impact activities that place excessive stress on the midfoot, such as running or jumping, may help manage symptoms.
In cases where these conservative measures are not effective, surgical intervention may be required.
Surgical Treatment
Surgery is considered when non-surgical treatments fail to provide adequate relief or when the symptoms of midfoot arthritis significantly impact daily activities. The goal of surgery is to reduce pain, restore foot function, and address deformities such as bone spurs.
- Midfoot Fusion (Arthrodesis): This procedure involves fusing the damaged joints in the midfoot to eliminate movement in the arthritic joints, thus relieving pain. Bone spurs may also be removed during the surgery to reduce rubbing against footwear. While fusion limits joint mobility, it can provide long-term relief from pain.
- Minimally Invasive Surgery: In some cases, it is possible to “work around” the problem by performing a minimally invasive procedure further down the foot to unload the painful area in the midfoot. This may be an option for patients with less severe arthritis or those who wish to avoid fusion.
Post-Surgical Care
Recovery from midfoot surgery typically involves a period of immobilization to allow the bones to heal. Patients may need to stay off the foot for several weeks, followed by gradual weight-bearing and physical therapy to restore strength and mobility. Full recovery can take several months, depending on the type of surgery performed.
Prevention of Midfoot Arthritis
While it is not always possible to prevent midfoot arthritis, certain measures can reduce the risk of developing the condition:
- Wearing supportive shoes that provide adequate cushioning and arch support.
- Maintaining a healthy weight to reduce stress on the joints.
- Avoiding high-impact activities that place excessive strain on the midfoot.
- Early treatment of foot injuries to prevent long-term damage to the joints.
Summary
Midfoot arthritis is a degenerative condition affecting the joints in the middle of the foot, leading to pain, stiffness, and difficulty with mobility. While non-surgical treatments such as supportive footwear, physiotherapy, and medications can help manage symptoms, surgery may be necessary for severe cases. With appropriate diagnosis and treatment, most individuals can achieve pain relief and restore function to the affected foot.